Research Article
Contextualizing COVID-19 Epidemiological Data: A Retrospective Study of Non-Hispanic Black American Seniors Living in Congregant Public Housing
885
Views & Citations10
Likes & Shares
Introduction: Non-Hispanic Black American (NHBA) seniors are dying at incredible rates from COVID-19 complications that appear related to health disparities and inequities. These factors increase transmissibility and hospitalizations of and for COVID-19 complications among NHBA seniors who live-in low-income congregant public housing
Methods: This cross-sectional retrospective study of 131 NHBA seniors and those living with mobility disabilities in congregant public housing used descriptive statistics to characterize participants.
Results: The mean age was 61.7 and 53% were female. Over a quarter had a mobility disability (28%) compares to those with no disability. Those with disabilities had higher prevalence of asthma (47%), diabetes (51%), hypertension (81%). Quality of life and social determinants of health were similar for each group.
Conclusion: While there was no statistically significant data, there were differences. Novel findings indicate, NHBA seniors living with a mobility disability were more susceptible to COVID-19 complications. They had a higher prevalence of hypertension, which is a significant indicator of COVID-19 hospitalizations. Adverse social and environmental determinants increased the threat of COVID-19 transmissibility. Findings also suggest they are more likely to suffer from lack of emotional and social support to help them cope with the pandemic.
Keywords: Non-Hispanic Black Americans, Seniors, Disabilities, COVID-19, Housing
INTRODUCTION
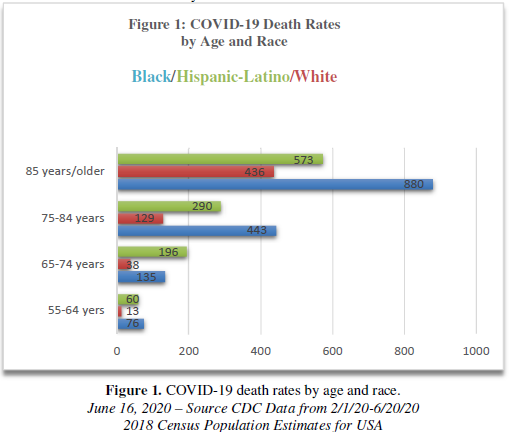
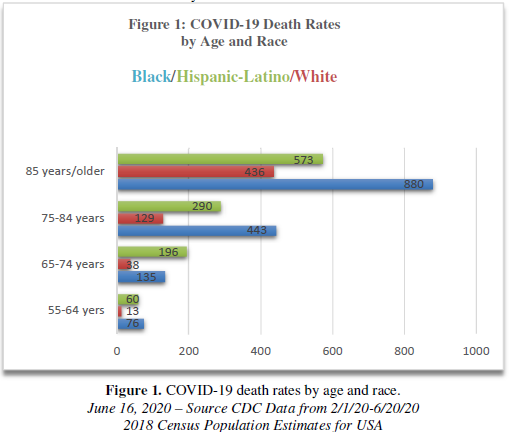
COVID-19 is devastating Non-Hispanic Black American (NHBA) communities across the United States (US) [1]. Overall, there is a disproportionate burden of COVID-19 morbidity and mortality among NHBAs compared to many Non-Hispanic ethnic groups in the US [1,2]. This predicament is especially perilous among NHBA seniors. There is high mortality toll among NHBA seniors represented in Figure 1 [3]. Forty-three percent have died from COVID19 compared to 16.6% of Whites. These numbers depict a dire situation for COVID-19 and NHBA seniors between the ages of 55-84+. There are large numbers of NHBA low-income seniors living in congregate public housing communities impacted by health disparities (<62 years old: 52.8%) [4], living within poor areas, and facing adverse social determinants with a heightened threat of COVID-19 [5-7]. There is a dearth of literature on NHBA seniors that characterize these health disparities and inequities (Figure 1).
As a result, this article presents descriptive epidemiological data to expose health disparities and inequities related to COVID-19 and NHBAs and seniors. It also includes a retrospective study with a sample of NHBA seniors living in congregant public housing to demonstrate the disproportionate burden of adverse social determinants, health disparities, and inequities they face as a result of their living conditions. This retrospective study provides findings that contextualize epidemiological data and demonstrates why NHBA seniors may have increased vulnerability to COVID-19 threats. Associations are outlined between current epidemiological data on COVID-19 and retrospective study findings. These nonstatistical correlations highlight how several factors aligned with the living conditions of NHBA seniors in congregant public housing may facilitate their higher risk to COVID-19 transmissibility and hospitalizations as represented in epidemiological data.
Epidemiological background
According to the National Health Interview survey, 2006-2012 [8], adults who live in the US Department of Urban and Housing Development (HUD)-assisted housing compared to the general adult US population are plagued by several chronic diseases: Higher prevalence of heart disease (19.8%; 12.8%, respectively), high blood pressure (37.9%; 26.5%, respectively), diabetes (17.6%; 9.5%, respectively), cancer (9.2%; 8.5%, respectively), chronic obstructive pulmonary disease (COPD; 13.1%; 6.1%, respectively), asthma (16.3%; 8.7%), respectively, 10+ days in bed (14.5%; 6.2%, respectively), and serious psychological distress (11.6%; 3.7%, respectively).HUD-assisted adult renters are 45% more likely to suffer from the aforementioned diseases and illnesses than the general population [8]. These data are striking considering several are listed as underlying medical conditions, increasing the risk of COVID-19, cancer, COPD, and heart conditions, asthma, high blood pressure, and Type 2 diabetes mellitus [9].
A COVID-19 diagnosis can come with relatively mild prognosis. However, for those with underlying conditions and seniors, the COVID-19 prognosis can be acute to lethal respiratory distress such as pneumonia, which can lead to acute respiratory distress syndrome and hospitalization [10]. Between March 1 and July 11, 2020 hospital rates NHBA seniors are 353.8 for 50-64 years and 743 for 65+ years. Sixty-five plus have the highest hospital rate across all other Non-Hispanic American ethnic/racial groups [9]. High Blood pressure leads as a chronic disease-causing highest percentage of COVID-19 hospitalizations across thirteen selected underlying conditions [9]. Compared to Non-Hispanic American Whites the prevalence of high blood pressure is highest in older NHBA males and females [9].
Health disparities and inequities
The evidence reveals that health disparities contribute to the accelerated decline in COVID-19 health outcomes among NHBA seniors. Generally, low-income NHBA seniors 65 years and older carry a disproportionate burden of chronic health conditions associated with poor outcomes from COVID-19, including hypertension, heart disease, chronic bronchitis or emphysema, and diabetes [11,12]. NHBAs who are 65 and older also have significantly higher co morbidity (2-4 or more) than across races and ethnicities [13-14]. Additionally, impoverished NHBA seniors are more likely to be less mobile [15]. NHBA seniors living with a mobility disability (LWMD) are at increased risk of unintentional injuries, high blood pressure, cardiovascular disease, diabetes, what also height has their risk of COVID-19 related complications [16,17]. These disparities are representative NHBA seniors who reside in congregant public housing and who face adverse social determinants of health and environmental factors, which are a result of systemic equities such as residential racial segregation.
Social determinants of health
Residential racial segregation characterized by majority-minority communities, create poverty pockets where NHBAs are more likely to be burdened with disease and faced with challenging environmental and social determinants. Racial residential segregation is associated with limited economic resources (household income <$14,000: 52%) [4,5]. Many do not have health insurance or regular access to health care [18,19]. More, these geographical regions are ground zero for the fight against COVID-19 [11,20,21]. Most public housing is in residential racially segregated neighborhoods.
Living in public housing is correlated with poor self-rated health and is identified as a fundamental cause of health disparities among Black Americans [20,22]. In particular, living in congregant public housing for NHBA seniors is characterized by a myriad of adverse environmental and social determinant health factors [13,14,19]. According to the CDC, the risks for severe COVID-19 illness are poverty [23]. These communities suffer from social isolation and little social attention; thus, adverse social determinants of health are left to thrive. Socially isolated low income Black American seniors living in public housing face poverty, limited access to services and resources, poor housing quality, and overcrowding [24,25,26]. According to the CDC, poverty and crowding are associated with risks for COVID-19 [23]. Additionally, the social determinants associated racial residential segregation can cause chronic stress which contributes to the ‘weathering’ or wearing down the physiology of seniors and seniors LWMD [24,25]. The 'weathering’ hypothesis increases the effect that physiological stress has on the body's ability to defend itself against disease, making NSBA seniors more vulnerable COVID-19 [24,25].
Most NHBA seniors live in apartment buildings with shared common spaces, elevators, staircases, mailrooms, hallways and laundry rooms where the coronavirus can exist for extended periods of time, facilitating transmission [27]. Further, complicating the manner, many seniors are not following CDC recommendations on social distancing and mask wearing [27,28]. Therefore, transmission dangers can rival the COVID-19 cases and deaths documented in US nursing homes [29]. There is evidence that the apartments occupied by Black American seniors are unhygienic, having mold, pest residue, and poor ventilation [30]. The CDC reports that proper ventilation is necessary for respiratory protection [31]. Not only are NHBA seniors’ health compromised by exposure to COVID-19 but health risks are compounded by exposure to air borne toxins due to poor ventilation.
The President of the National Alliance of The Department of Housing and Urban Development (NAHUD) Tenants points out that deaths are rampant in the senior buildings. Ambulances are commonplace on site; residents are dying but other residents are unaware of the cause [27]. There no HUD regulations to report cases or inform residents, there are no safeguards in place to protect the other residents, and no oversight [32]. With most seniors having chronic diseases and high co-morbidities, they live under conditions in which are exposed to COVID-19 transmission, are susceptible to COVID-19 health complications, and some even die along in their apartments due to mobility disabilities.
A retrospective study
The following retrospective study took place in the fall of 2018. While this investigation occurred prior to the COVID-19 outbreak, it has not been published and is no less significant. This investigative study is necessary to understand the context lived in by NHBA seniors in congregant public housing. Therefore, the following study focused on investigating chronic disease status, health risk behaviors, quality of life and the social determinants of health impacting NSBA seniors and those with limited mobility disabilities who live in congregant public housing in low income neighborhoods. The aim of this retrospective study is to contextualize current epidemiological data within the health and lives of NHBA living in congregate public housing.
METHODS
Ethics review
Rutgers University's School of Information and Communication funded this research. The study protocol was approved and monitored by the Institutional Review Board at Rutgers University. There are no conflicts to disclose. All assistants and researchers are CITI Certified.
Recruitment
The study took place in collaboration with a public housing community in a midsized city in the US Northeast with approximately 3200 residents, 29% were between ages 55-98. Recruitment involved using flyers and advertisements at the three senior housing properties; however, it was primarily executed by word-of-mouth.
Eligibility requirements
To participate in the study, residents had to live in one of the three senior housing properties; between the ages of 55-85 living with a mobility disability (LWMD) or without a mobility disability; and self-identify as Non-Hispanic African American or Black American.
Recruitment environment
The author has worked closely with the NHBA seniors at this public housing authority for years. The environment is unchanged since 2014, The three public housing senior properties from which the NHBA seniors were recruited are high rises located within racially residential segregating urban communities that are highly disordered with crime, gun violence, drug dealing, drug addicts, drunks, and liquor stores. There are no grocery stores near senior buildings, only bodegas (corner stores). Each high rise has structural flaws, an institutional warehouse feels, and only two elevators per building. Usually, one elevator works at a time, with individuals having to crowd into one elevator. Repairs are inadequate (e.g., painting over black mold). On-site supportive health services exist for short periods or not at all; thus, many NHBA seniors do not know about them. The majority of the NHBA seniors and those LWMD are poverty-stricken, stressed, and fearful of the administration evicting them for speaking out about problems with their apartment or housing conditions in general. Some seniors are living in social isolation, and many are resigned to the poor condition of just surviving.
Data collection
This study used a non-probability sample. Data collection took place in the community rooms of each of the three sites. Three focus groups with 15 participants each were held at each senior site were used to administer the survey. The informed consent was read aloud, and each person wanting to participate signed the consent form, which was collected by a CITI Certified Community Health Worker (CHW). The Principal Investigator (PI; i.e., author) distributed the surveys and, with the help of the CHW, assisted participants with literacy and sighted challenges. After reviewing the survey to ensure all answers to all questions, the PI provided each participant with a $35 cash incentive.
Questionnaire
A close-ended questionnaire collected information on the presence of chronic conditions, health-related outcomes, and quality of life. Questions came from the US Behavioral Risk Factor Surveillance System Questionnaire (BRFSS) for demographic (e.g., age, sex, marital status, education level, and household income), health-related questions (e.g., presence of health conditions and healthcare utilization), health behaviors (e.g., smoking status), and social determinants (e.g., food security, financial security, and chronic stress) [33]. Questions on health and functioning were from the US Short Form Health Survey (SF-36) [34]. This instrument measures physical vitality functioning, bodily pain; general health perceptions; physical role functioning; emotional role functioning; social role functioning, and mental health. The SF-36 is a valid and reliable instrument for use with NHBA seniors and seniors LWMD [35,36]. Quality of life was measured using the World Health Organization Quality of Life Brief Version (WHOQOL-BREF) scale, a valid and reliable instrument measures physical health, psychological health, social relationships, and environment [37].
Data analysis
Data from sample populations of all three public housing facilities were integrated in this report to ensure an adequate sample size. Descriptive statistics computed survey questions using SAS Software [38]. Statistics were organized based on disability status - those having a self-reported mobility disability compared to those who did not have a self-reported mobility disability. Means and standard deviations described continuous variables for each group. Frequencies described categorical variables. Independent sample t-tests or Wilcoxon tests compared the means of continuous variables for PLWD-mobility and those without a mobility disability; chi-square tests determined the relationship between categorical variables. The level of statistical significance was p<0.05.
RESULTS
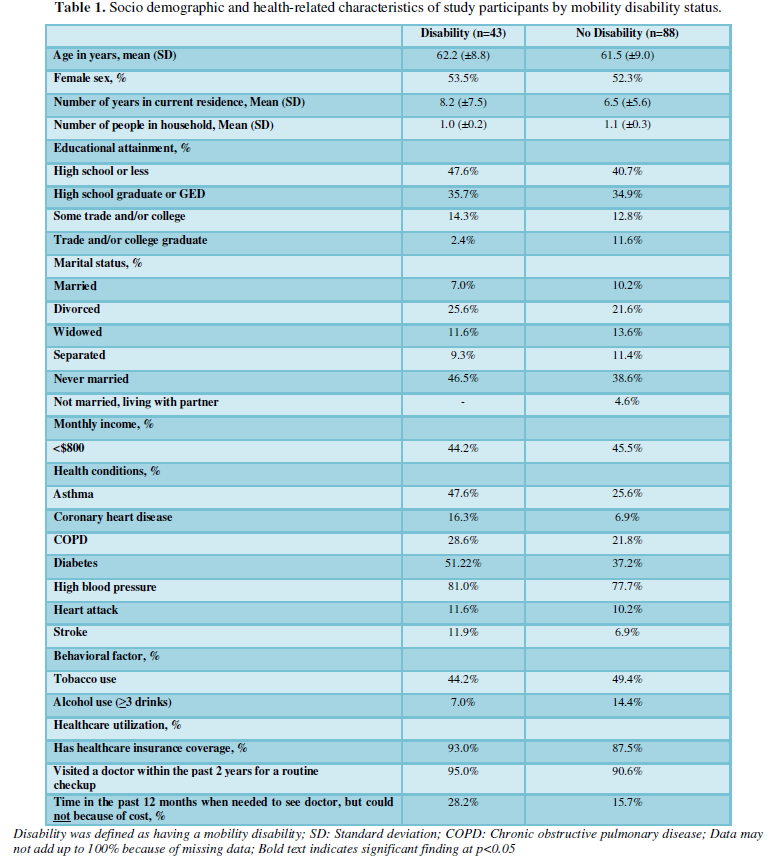
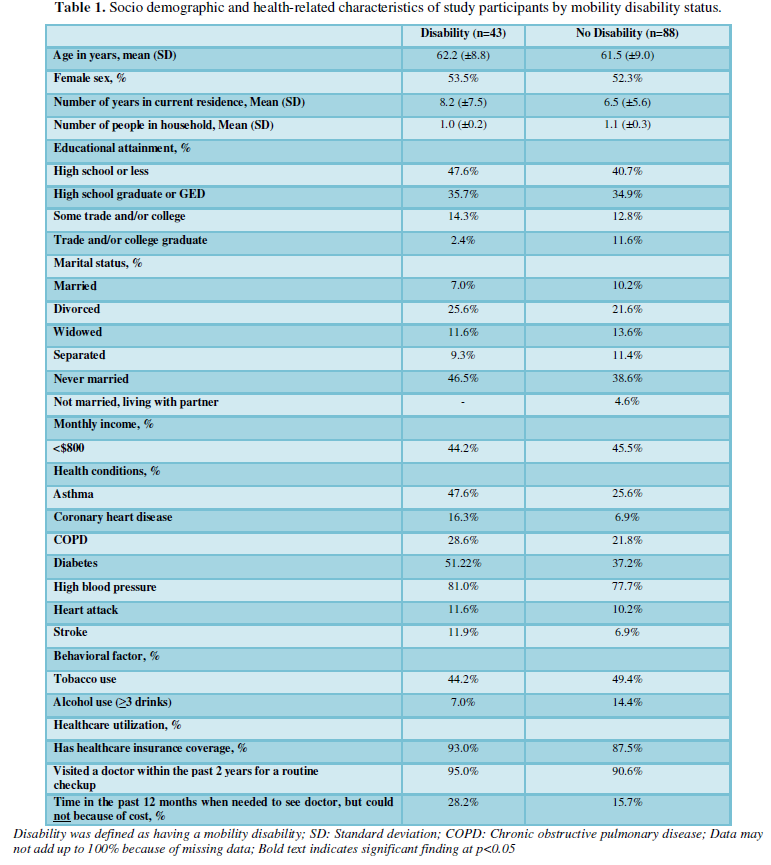
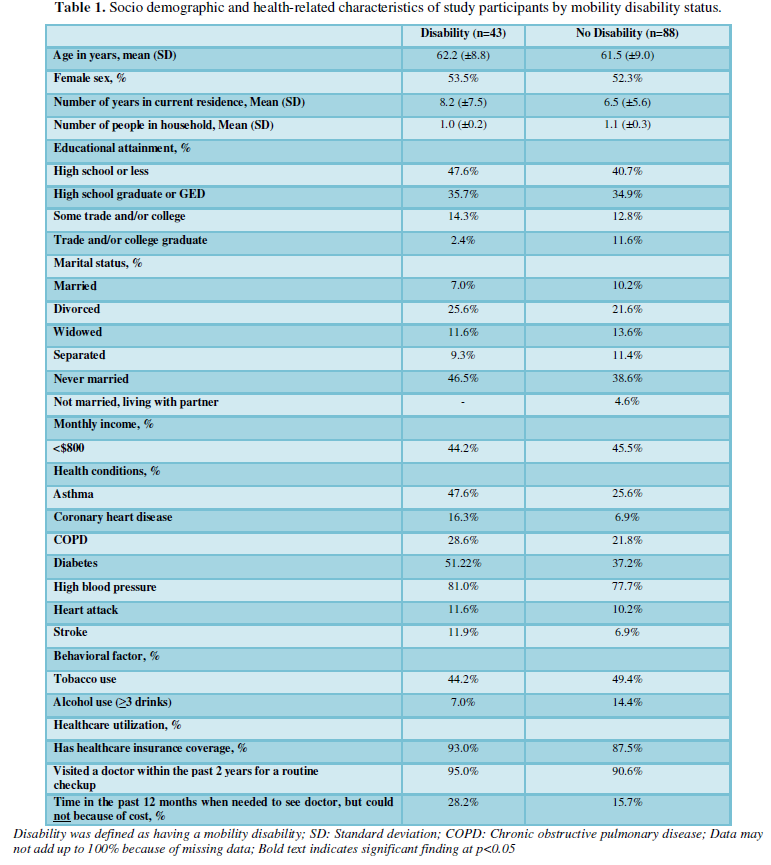
Out of one hundred and thirty-five surveys (135), one hundred and thirty-one (131) participants were eligible for data analysis, of which 33% self-reported having a mobility disability (n=43l (Table 1). There were no statistically significant differences in demographic characteristics between seniors living with a mobility disability (LWMD) and those without LWMD. The mean age for both groups was about 62 years, and there was a similar sex distribution, with more than half of respondents being female for both groups. The proportion of participants who reported a monthly income below $800 was similar for both groups (44.2% and 45.5%).
The presence of health conditions was similar for both groups, except for asthma; seniors LWMD had a significantly higher prevalence of asthma than those without a mobility disability (47.6% and 25.6%, respectively). The prevalence of high blood pressure was high for seniors LWMD and those without (81.0% and 77.7%), followed by diabetes (51.22% and 37.2%) and chronic obstructive pulmonary disease (COPD) (51.22% and 37.2%). There were also no significant differences between seniors LWMD and those without tobacco use (44.2% and 49.4%, respectively) or alcohol use (7.0% and 14.4%, respectively). Both groups reported having a similar prevalence of healthcare insurance coverage (93.0% and 87.5%) and having visited a healthcare provider in the past 12 months.
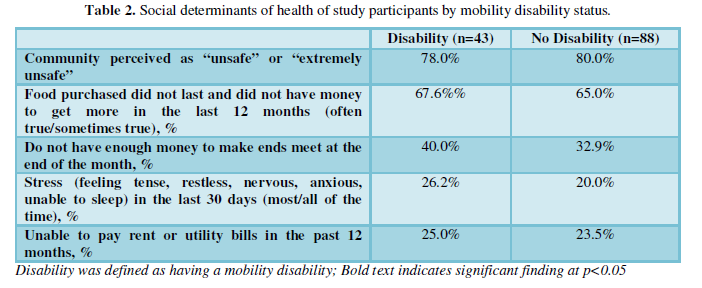
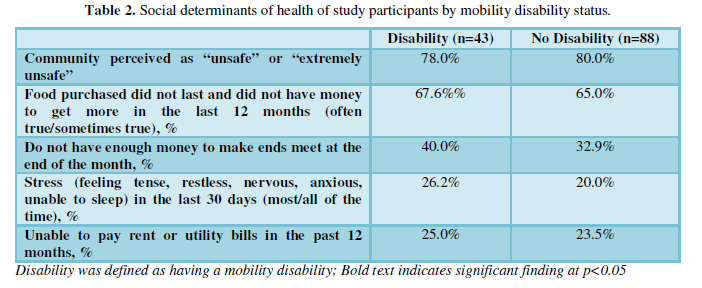
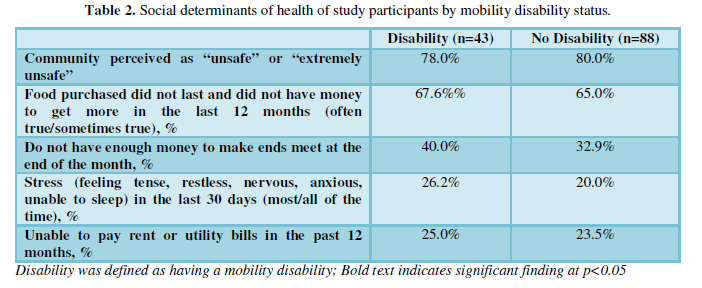
The presence of adverse social determinants was high for both seniors LWMD and those without mobility disability (Table 2). All participants perceived their community as “unsafe” or “extremely unsafe” (78.0% and 80.0%). Both seniors LWMD and those without a mobility disability reported high levels of food insecurity at some point in the past 12 months by stating that the following statement was “often true” or “sometimes true”: “The food that I bought just didn't last, and I didn't have money to get more” (67.6% and 65.0%, respectively). A higher proportion of seniors LWMD reported financial insecurity, that is, s/he did not “have enough money to make ends meet at the end of the month”. Seniors LWMD reported slightly higher levels of stress than those without a mobility disability; however, it was not statistically significant (26.2% and 20.0%). Also, participants in both groups reported being unable to pay rent or utility bills within the past year (25.0% and 23.5%).
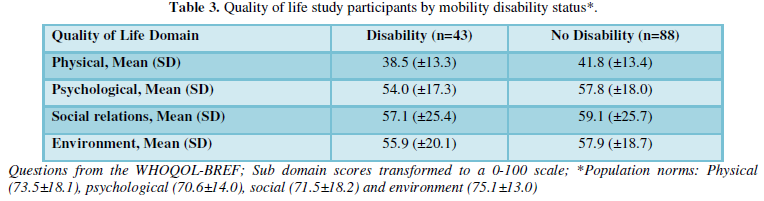
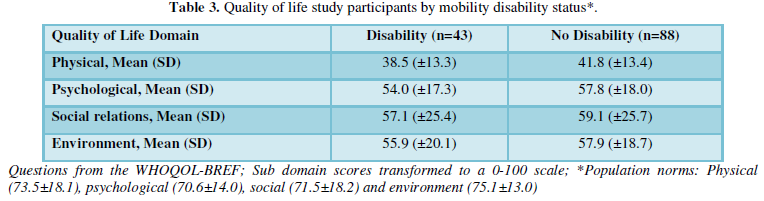
There were no statically significant differences in quality of life measures between seniors LWMD and those without mobility disability. Participants reported similar quality of life outcomes for the physical domain (38.5±13.3 and 41.8±13.4), psychological domain (54.0±17.3 and 57.8±18.0), social relations domain (57.1±25.4 and 59.1±25.7), and environment domain (55.9±20.1 and 57.9±18.7). These scores were lower than the population norm averages (Table 3).
DISCUSSION
This investigation is the first retrospective study to examine differences in demographic and health-related characteristics among seniors and seniors LWMD living in congregate public housing who self-identify as Black/African American in order to contextualize COVID-19 epidemiological data to establish if their health and mobility status as well as living conditions places them at higher risk for COVID-19 transmissibility and hospitalizations [1-3]. Not surprisingly, there were no statistically significant differences across demographic and health-related characteristics between NHBA seniors LWMD and those without a mobility disability. This is more than likely due to living in similar geographic regions and neighborhoods with dealing with the same socio environmental challenges. However, there were differences. This study reveals that NHBA seniors LWMD are at higher risk for COVID-19 morbidity and mortality.
COVID-19 and seniors LWMD
Applying this study to the COVID-19 pandemic reveals significant challenges for those seniors LWMD. In the present study, NHBA seniors LWMD reported a higher prevalence of chronic diseases and poorer overall health compared to those without mobility disabilities, which increases their risk for COVID-19 complications. These findings support research reporting that NHBA seniors in public housing are more likely to have a chronic disease and rate their health as fair or poor [8,11,13, 22]. Our findings also demonstrate that NHBA seniors LWMD see their physician on a more regular basis than those without disability mobility. This access aligns National Surveillance Data reports [39]. However, COVID-19 is a disruptive factor in access to health care.
When it comes to testing for the COVID-19 virus in United States (US) the individual must provide a physician prescription or be symptomatic to qualify for COVID-19 testing. If there is no prescription, there are areas in the US where individuals must stand in long lines to get tested if they do not have a car. These rules create challenges for NHBA senior LWMD [17]. More, CDC guidelines are clear on social distances [28]. Currently, most physician see patients remotely. Generally, low income NHBA seniors may not have access to or not know how to use technology. Thus, remote connectivity with physicians may not occur as needed, impacting their health and well-being.
While chronic disease outcomes in NHBA seniors LWMD is due to many factors (e.g., no physical activity), emotional support as a protective factor [40,41]. Emotional support is Social support, important to emotional well-being, is impacted by the COVID-19 outbreak [42]. In the present study NHBA seniors LWMD reported a higher prevalence of stress than those without a mobility disability. They also reported greater financial insecurity. Stress can partly be explained by reported financial insecurity among seniors with mobility disabilities. However, COVID-19 compounds stress through worry over disruptions in daily life [42]. Disruptions can increase worries over financial stability in turbulent times. Due to social distancing policies, NHBA seniors living with a mobility disability may not experience the same type or degree of emotional and social support experienced prior to COVID-19.
Studies report increases in COVID-19 related anxiety depression, and stress [43,44]. The current study found that those NHBA seniors LWMD scored lower on having social relations than the general population. Stress is increased through disruptions in social support, which can perpetuate emotional turmoil and erode adaptive coping skills in times of disaster, leading to psychological distress [42]. Social support can ameliorate maladaptive emotions and coping skills fostered by the pandemic. Mover, disaster-related stress aggravates hypertension. NHBA seniors LWMD reported higher levels of stress and hypertension than those without mobility disabilities. Hypertension is the cause of the highest COVID-19 hospitalization rates among seniors [9,16,17].
LIMITATIONS
There are several limitations to this study. The study focused on one public housing authority in three senior designated properties. Therefore, insignificant findings may be due to all the seniors similarly experiencing the same realities. The findings related to purposeful sampling may not be generalizable to other NHBA seniors and those LWMD from public housing authorities. There may also be an element of social desirability impacting participants' answers to the questions. Desirability seems to be particularly evident in the question concerning the use of alcohol. With the author having worked with the seniors and those with disabilities for over five years, the use of alcohol occurred across sites. Additionally, the cash incentive may have motivated participants to fill out the questionnaires as fast as possible without considering the questions to obtain the incentive. There was also the issue of literacy and sighted disabilities that caused challenges in tracking and answering questions, even though there was a CITI certified Community Health Worker assisting participants. Lastly, the focus group format possibly provided participants the opportunity to collude in copying survey answers. These limitations, however, do not distract from the more significant health implications impacting NHBA seniors living in public housing authorities and the possibility of an all-out COVID-19 outbreak based on literature and data presented in this paper.
CONCLUSIONS
While there were no significant differences between NHBA seniors LWMD and those living without, there were notable differences. NHBA seniors with LWMD were at higher risk for COVID-19 morbidity and mortality because they had a higher prevalence of chronic disease, suffered greater financial insecurities and had a lower quality of life than compared to the general population More these adverse social determinants tied to residential racial segregation caused a weathering effect and stress level that exacerbates chronic disease. Additionally, there were disruptions to social support and regular physician visitation caused by the pandemic. NHBA seniors LWMD were at increased risk for transmission of the virus and hospitalizations due to living in congregant public housing residences. Clearly, it is time to reexamine these health disparities and inequities among NHBA seniors LWMD bought to light by COVID-19 and this study. NHBA seniors living in congregant public housing require greater public health attention and on-site clinical treatment to which they have the right.
-
Centers for Disease Control and Prevention (2020) Weekly update by selects demographic and geographic characteristic. Available online at : https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm
-
APM Research Lab (2020) The color of coronavirus : COVID-19 deaths by race and ethnicity in the US. Available online at : https://www.apmresearchlab.org/covid/deaths-by-race
-
Centers for Disease Control and Prevention (2020) National Center for Health Statistics. Available online at : https://www.cdc.gov/nchs/index.htm
-
National Center for Health in Public Housing (2016) Demographic facts of resident living in public housings. Available online at : https://nchph.org/wp-content/uploads/2016/07/Demographics-Fact-Sheet-2016.pdf
-
Docter B, Galvez M (2020) The future of public housing fact sheet. Urban Institute.
-
Yancy CW (2020) COVID-19 and African Americans (published online ahead of print). JAMA 10 : 1001.
-
Applegate WB, Ouslander JG (2020) COVID‐19 presents high risk to older persons. J Am Geriatr Soc 68(4): 681.
-
Helms VE, Sperling J, Steffen BL (2017) A health picture of HUD-assisted adults, 2006-2012 : HUD administrative data linked with the national health interview survey. US department of housing and urban development, Office of Policy Development and Research.
-
CDC (2020) COVID View Weekly Survelliance Summary of U.S COVID-19 Activity. Available online at : https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
-
Wynants L, Van Calster B, Bonten MM, Collins GS, Debray TP, et al. (2020) Prediction models for diagnosis and prognosis of COVID-19 infection: Systematic review and critical appraisal. BMJ 369.
-
Lackland DT (2014) Racial differences in hypertension: Implications for high blood pressure management. Am J Med Sci 348(2): 135-138.
-
Centers for Disease Control and Prevention (2020) Information for Health Departments on reporting cases of COVID-19. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/php/reporting-pui.html
-
Golden SH (2020) Coronavirus in African Americans and other people of color. Johns Hopkins Medicine Health 2020.
-
Older Adults Healthy People (2020) Available online at: https://www.healthypeople.gov/2020/topics-objectives/topic/older-adults
-
Daw J (2017) Contribution of four comorbid conditions to racial/ethnic disparities in mortality risk. Am J Health Promot 52(1): S95-S102.
-
Ward BW, Schiller JS (2013) Peer reviewed: Prevalence of multiple chronic conditions among US adults: Estimates from the National Health Interview Survey, 2010. Prev Chronic Dis 10.
-
Grant TL, Edwards N, Sveistrup H (2010) Inequitable walking conditions among older people : Examining the interrelationship of neighborhood socio-economic status and urban form using a comparative case study. BMC Public Health 10(1): 677.
-
Anderson LL, MapelLentz S, Larson SA (2019) Physical disability and health disparities. Advances in Exercise and Health for People with Mobility Limitations, pp: 41-59.
-
Satariano WA, Guralnik JM, Jackson RJ, Marottoli RA, Phelan EA, et al. (2012) Mobility and aging: New directions for public health action. Am J Pub Health 2(8): 1508-1515.
-
Martin P, Liaw W, Bazemore A (2019) Adults with housing insecurity have worse access to primary and preventive care. J Am Board Fam Med 32(4): 521-530.
-
Ahmed SM, Lemkau JP, Nealeigh N, Mann B (2001) Barriers to healthcare access in a non‐elderly urban poor American population. Health Soc Care Commun 9(6) : 445-453.
-
Williams DR, Lawrence JA, Davis BA (2019) Racism and health: Evidence and needed research. Annu Rev Public Health 40 : 105-125.
-
Ruel E, Oakley D, Wilson GE, Maddox R (2010) Is public housing the cause of poor health or a safety net for the unhealthy poor? J Urban Health 87(5) : 827-838.
-
Priest N, Williams DR (2018) Racial discrimination and racial disparities in health. The Oxford Handbook of Stigma, Discrimination and Health. Oxford Library of Psychology Online.
-
Centers for Disease Control and Prevention (2020) People who are at higher risk for severe illness. Coronavirus Disease (COVID-19). Available online at : https://www.cdc.gov/coronavirus/2019-ncov/need-extra precautions/people-at-higher-risk.html
-
Fiorati RC, Elui VM (2015) Social determinants of health, inequality and social inclusion among people with disabilities. Rev Lat Am Enfermagem 23(2) : 329-336.
-
Harley AE, Yang M, Stoddard AM, Adamkiewicz G, Walker R, et al. (2014) Patterns and predictors of health behaviors among racially/ethnically diverse residents of low-income housing developments. Am J Health Promot 29(1) : 59-67.
-
Williams DR, Collins C (2016) Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Rep 116(5): 404-416.
-
Graham (2020) Seniors in low-income housing live in fear of COVID Infection. Available online at: https://khn.org/news/seniors-in-low-income-housing-live-in-fear-of-covid-infection/
-
CDC (2020) How to protect yourself and others. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
-
Barnett ML, Grabowski DC (2020) Nursing homes are ground zero for COVID-19 pandemic. JAMA 1: e200369-e200369.
-
The Department of Housing and Urban Development (HUD) (2020) Housing-related health and safety hazards assessment. Available online at: https://www.hud.gov/sites/documents/HHPGM_FINAL_CH4.PDF
-
CDC (2020) COVID-19 Employer information for office buildings. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/community/office-buildings.html
-
COVID-19 (2020) Frequently asked questions (FAQs) for public housing authorities, version 3.
-
Behavioral Risk Factor Surveillance System (2017) Centers of Disease Control and Prevention. Available online at: https://www.cdc.gov/brfss/data_documentation/index.htm
-
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6): 473-483.
-
Cernin PA, Cresci K, Jankowski TB, et al. (2010) Reliability and validity testing of the short-form health survey in a sample of community-dwelling African American older adults. J Nurs Meas 18(1): 49-59.
-
Syddall HE, Martin HJ, Harwood RH, et al. (2009) The SF-36: A simple, effective measure of mobility-disability for epidemiological studies. J Nutr Health Aging 13(1): 57-62.
-
Skevington SM, Lotfy M, O'Connell KA, Cooper C, Sayer AA (2004) The World Health Organization's WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 13(2): 299-310.
-
SAS Institute Inc. (2014) SAS Version 9. Cary, NC: SAS Institute Inc., 2014.
-
Havercamp SM, Scott HM (2015) National health surveillance of adults with disabilities, adults with intellectual and developmental disabilities and adults with no disabilities. Disabil Health J 8(2): 165-172.
-
Heim C, Ehlert U, Hellhammer DH (2000) The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 25(1): 1-35.
-
Reblin M, Uchino BN (2008) Social and emotional support and its implication for health. Curr Opin Psychiatr 21(2): 201-205.
-
Park CL, Russell BS, Fendrich M, Finkelstein FL, Hutchison M, et al. (2020) Americans’ COVID-19 stress, coping and adherence to CDC Guidelines. J Gen Intern Med 35 (8): 2296-2303.
-
Pfefferbaum B, North CS (2020) Mental health and the COVID-19 pandemic. N Engl J Med 383 (6): 510-512.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Allergy Research (ISSN:2642-326X)
- Advance Research on Alzheimers and Parkinsons Disease